
Oftalmika Eye Clinic
Offers
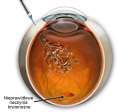
CATARACT
 Cataract is opacity in the eye lens causing blurred and distorted vision. The disease is painless and its frequency of appearance grows with age.
Cataract is opacity in the eye lens causing blurred and distorted vision. The disease is painless and its frequency of appearance grows with age. The most common symptoms of cataract:
- cloudy vision;
- vision deterioration in dim light, e.g. in the evening;
- the necessity to use stronger light while reading;
- double vision in a single eye;
- matt perception of colours;
- the necessity of very frequent change of glasses;
- diffusion of lights;
Cataract operation can be performed at any time and it is independent of the patient’s age.
Treatment
 The only efficient method of treatment is an operation. The indication for the surgery is vision deterioration which disturbs the patient’s everyday activities and is independent of their age. The operation consists in extraction of the opaque lens and implanting an artificial one in its place.
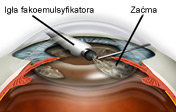
The only efficient method of treatment is an operation. The indication for the surgery is vision deterioration which disturbs the patient’s everyday activities and is independent of their age. The operation consists in extraction of the opaque lens and implanting an artificial one in its place. In our clinic the operation lasts several minutes and the patient stays at the clinic only a few hours. The surgery is performed under topical anaesthesia, which prevents the patient from feeling the pain. At the beginning we perform some small incisions, which makes the healing process possible to take place quickly and without stitches. For removing cataract masses we apply a state-of-the-art Swiss phacoemulsificator. We use materials of the highest quality and we implant well-tried artificial lenses.
With extra payment it is possible to: 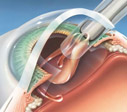
- implant the most technologically advanced artificial lenses produced by an American company Alcon (ArcySof Natural, Acrysof IQ and a pseudoaccommodation lens Restor);
- perform an even smaller incision, microincision of about 2,2mm, to further improve the healing process and diminish the postoperational astigmatism;
- be accommodated in a single room with a possibility of being accompanied by a relative;
Only in our clinic our patients are offered a possibility of a simultaneous astigmatism correction by using limbal relaxing incisions. It is a recognized technique in the world but still not very popular in Poland. The use of suitable incisions by means of a diamond knife makes it possible to reduce astigmatism even by 3 dioptres. The use of limbal relaxing incisions improves refractive results of cataract surgery, which in turn involves weaker or no glasses at all for the patient.
Remember: 

- it’s no use procrastinating cataract surgery, for the patient’s comfort and medical reasons it is better to operate when it starts to disturb you;
- after the artificial lens implantation it is necessary to wear glasses for far and near vision, only Restor lens makes it possible to live without the necessity of wearing glasses;
- once removed, cataract never comes back.
About 20% of patients within a few years after the operation develop the opacification of the posterior capsule which remained in the eye (secondary cataract). This opacification can be removed by means of a suitable laser (capsulotomy). The surgery lasts several minutes and is performed at our clinic as an outpatient service.
Artificial lenses implanted after the cataract removal: 

- AcrySof®Natural – it has a yellow filter imitating the natural colour of the lens which diminishes the negative influence of blue light on the retina;
- AcrySof®ReSTOR®IQ – a multifocal lens, enables far and near vision after the cataract surgery without the necessity of wearing glasses;
- AcrySof®IQNatural – besides the yellow filter it has an aspherical construction which improves the quality of vision
Patient’s preparation:
Before the qualification visit the following examinations should be carried out: blood morphology, APTT, HBS, HCV, Ekg. Then the patient is examined by an ophthalmologist and an anaesthesiologist and the surgery is scheduled. The patient is informed how to prepare for the operation.
- to provide the patient with full comfort and safety their general condition is monitored by an anaesthesiologist throughout the whole surgery;
- the patient to be operated does not have to be on an empty stomach, though it is advisable not to eat any meals within a few hours before arrival at the clinic;
- patients with diabetes should stick to their normal rhythm of meals and insulin therapy;
- before the operation the patient should not change the dosage of medications they take on everyday basis;
- drugs ‘thinning’ blood should not be used within 7 days before the planned surgery after a consultation with an internist (i.e.: Acard, Acenokumarol, Polocard, Bestpirin);
- 2 days before the planned surgery the patient should use the following drops (administered into the operated eye)
- 0,5% Oftensin – 2 times a day
- antibiotic drops (i.e: Oftaquix) – 4 times a day
- 5 hours before the arrival at the clinic - 2 tablets of Cyclonamine
- just before leaving home 1% Tropicamid drops 2 times to the eye within 10 minute intervals;
- on the day of the surgery the patient should wear comfortable clothes, take pyjamas or a nightgown and a small towel. It is advisable to arrive accompanied by a relative or a friend. The expected time of stay at the clinic: up to 4 hours.
After the surgery:
- the operated eye dressing should remain in its place until the first control visit;
- after the first ophthalmological examination proper eye drops will be prescribed and the date of the following visit will be planned;
- within the first 2-3 weeks after the surgery great physical effort should be avoided;
- avoid pressing or rubbing the operated eye;
- watching TV or reading are allowed;
- after 24 hours the patient can stop using the eye dressing in enclosed areas, hair washing is allowed yet special care should be taken to prevent the shampoo from getting into the operated eye;
- until the time of the prescription of new glasses (1 month after the operation) the former ones can be used.
RETINA DISEASES
 Retina is a thin, transparent tissue which makes the inner layer of the eyeball wall. It contains photosensitive cells and is able to receive light stimuli. The central part of the retina is called the macula, and the diseases of that region of the eyeball – macular diseases. They can be caused by blood vessels damage, inflammations, injuries, cancer, or may have genetic bases. The most frequent disease of the macula is age-related macular degeneration (AMD) caused by the damage of the retinal pigment epithelium, which in turn, results from chronic inflammation induced by deposits of lipofuscin accumulated throughout the whole life. The disease occurs in two forms. The mild one, so called: dry (non-exudative) AMD is connected with the appearance of areas of retina atrophy and slow deterioration of visual acuity. In wet (exudative) AMD new, diseased, leaking and fragile blood vessels grow outwards under the retina causing fast sight deterioration. Another frequent retina disease is diabetic retinopathy. At first the disease brings about the damage of tiny retinal vessels, which results in inadequate blood supply in some areas. This, in turn, causes retinal vessels proliferations accompanied by recurrent bleeding and tractional retinal detachment.
Retina is a thin, transparent tissue which makes the inner layer of the eyeball wall. It contains photosensitive cells and is able to receive light stimuli. The central part of the retina is called the macula, and the diseases of that region of the eyeball – macular diseases. They can be caused by blood vessels damage, inflammations, injuries, cancer, or may have genetic bases. The most frequent disease of the macula is age-related macular degeneration (AMD) caused by the damage of the retinal pigment epithelium, which in turn, results from chronic inflammation induced by deposits of lipofuscin accumulated throughout the whole life. The disease occurs in two forms. The mild one, so called: dry (non-exudative) AMD is connected with the appearance of areas of retina atrophy and slow deterioration of visual acuity. In wet (exudative) AMD new, diseased, leaking and fragile blood vessels grow outwards under the retina causing fast sight deterioration. Another frequent retina disease is diabetic retinopathy. At first the disease brings about the damage of tiny retinal vessels, which results in inadequate blood supply in some areas. This, in turn, causes retinal vessels proliferations accompanied by recurrent bleeding and tractional retinal detachment. Diagnostics
 Apart from stereoscopic evaluation of the macula by means of Volka lens we perform fluorescein angiography as a routine procedure. It consists in intravenous administration of a substance called: fluoroscein. It is a kind of dye capable of being fluorescent. Under the influence of violet-blue light it emits yellow-green radiation which is recorded by a digital camera being a part of a device called: fundus camera – used for taking retina images. Fluorescein noted on arterial, venous and capilliary veins of the retina is recorded in frames. Every damage and new vessels growing from the retina and the choroid can be seen in this way. Another method of the retina examination is Spectral Optical Coherent Tomography (SOCT). The device records reflections of light from particular layers of the retina making it possible to acquire cross sections of that tissue slightly resembling histological preparations. It is the most modern way of macular diagnostics allowing to detect even small changes which are still not detectable in fluorescein angiography.
Apart from stereoscopic evaluation of the macula by means of Volka lens we perform fluorescein angiography as a routine procedure. It consists in intravenous administration of a substance called: fluoroscein. It is a kind of dye capable of being fluorescent. Under the influence of violet-blue light it emits yellow-green radiation which is recorded by a digital camera being a part of a device called: fundus camera – used for taking retina images. Fluorescein noted on arterial, venous and capilliary veins of the retina is recorded in frames. Every damage and new vessels growing from the retina and the choroid can be seen in this way. Another method of the retina examination is Spectral Optical Coherent Tomography (SOCT). The device records reflections of light from particular layers of the retina making it possible to acquire cross sections of that tissue slightly resembling histological preparations. It is the most modern way of macular diagnostics allowing to detect even small changes which are still not detectable in fluorescein angiography. Preparation for retina examination.
 In order to precisely evaluate the condition of the retina, it is necessary to dilate the pupil. It is connected with sight deterioration lasting for 2-3 hours involving the preventive inability to drive a car. In the case of fluorescein angiography injection in the vein under the elbow takes place. After administering fluorescein, temporary nausea may appear, and in patients allergic to iodine contrastive substances, more serious allergic reactions may be expected. After the examination, the skin temporarily acquires yellow colour. SOCT examination is not connected with taking any medications, so there is no risk of unwanted reactions.
In order to precisely evaluate the condition of the retina, it is necessary to dilate the pupil. It is connected with sight deterioration lasting for 2-3 hours involving the preventive inability to drive a car. In the case of fluorescein angiography injection in the vein under the elbow takes place. After administering fluorescein, temporary nausea may appear, and in patients allergic to iodine contrastive substances, more serious allergic reactions may be expected. After the examination, the skin temporarily acquires yellow colour. SOCT examination is not connected with taking any medications, so there is no risk of unwanted reactions. Treatment
Laser therapy – a laser ray causes the phenomenon of photocoagulation, i.e.: a strong thermal effect localised in a small area which causes the damage of the outer layers of the retina. This kind of therapy is especially effective in treatment of diabetic retinopathy, conditions following retina blood vessels clotting and other diseases of vascular origins. In the case of small changes we perform focal therapy whose aim is direct destruction of the damaged fragments of the fundus blood vessel system. If the changes are more advanced, scatter laser photocoagulation is used covering the spread area of the leakage with foci of the chessboard layout. In the case of eyes with proliferative retinopathy, it is necessary to perform panphotocoagulation. Although laser surgeries of that type can be performed with lasers of different wavelength, the most common procedure is to use the laser emitting green light (532 nm).
 Intraviteral injections of drugs hindering vessel growth are the latest and most efficient methods of treatment of the wet form of AMD and other macular diseases in which there appears growth of the pathological blood vessels. The first registered drug of that type is pegaptanib (Macugen), the second – ranibizumab (Lucentis). The third one – bevacizumab (Avastin) hasn’t been registered for intraviteral injections, but has been used commonly all over the world. All of them work similarly by blocking substances stimulating growth of the vessels’ endothelium. Clinical research proves that administering Lucentis or Avastin every 4 weeks improves the vision of the majority of patients in all kinds of subretinal neovascularisation in AMD.
Intraviteral injections of drugs hindering vessel growth are the latest and most efficient methods of treatment of the wet form of AMD and other macular diseases in which there appears growth of the pathological blood vessels. The first registered drug of that type is pegaptanib (Macugen), the second – ranibizumab (Lucentis). The third one – bevacizumab (Avastin) hasn’t been registered for intraviteral injections, but has been used commonly all over the world. All of them work similarly by blocking substances stimulating growth of the vessels’ endothelium. Clinical research proves that administering Lucentis or Avastin every 4 weeks improves the vision of the majority of patients in all kinds of subretinal neovascularisation in AMD. Preparation of the patient for an injection.
Macugen, Lucentis, and Avastin are administered into the eye in the form of injections which are given in the operational theatre. For three days preceding the injection the patient should take antibiotic drops 3 times a day. Just before an injection, drops causing pupil dilation as well as anaesthetic drops are used. The main drug administration lasts about 5 minutes. Half an hour later, after the ophthalmic examination and intraocular pressure taking, the patient goes home with an instruction to take antibiotic drops for three days after the surgery.
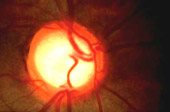
GLAUCOMA
 Glaucoma is a group of diseases whose common feature is chronic, progressing damage to the optic nerve reflected in the changes of the appearance of the optic disc accompanied by depletion in the field of vision. The most common type is primary open-angle glaucoma, which affects people after 40 years of age and is characterised by asymptomatic development leading to irreversible blindness. The most important risk factors include: age, glaucoma appearing in the family and myopia. Much more rarely can we find primary closed-angle glaucoma. It is connected mainly with hyperopic eyes with acute angle closure in which there appear conditions for its temporary closure. In such a situation, intraocular pressure rises considerably and there appear symptoms of glaucoma acute attack dominated by strong headache and pain in the eye. Another common type of glaucoma is secondary glaucoma accompanying other eye diseases, such as inflammations, injuries or diabetes.
Glaucoma is a group of diseases whose common feature is chronic, progressing damage to the optic nerve reflected in the changes of the appearance of the optic disc accompanied by depletion in the field of vision. The most common type is primary open-angle glaucoma, which affects people after 40 years of age and is characterised by asymptomatic development leading to irreversible blindness. The most important risk factors include: age, glaucoma appearing in the family and myopia. Much more rarely can we find primary closed-angle glaucoma. It is connected mainly with hyperopic eyes with acute angle closure in which there appear conditions for its temporary closure. In such a situation, intraocular pressure rises considerably and there appear symptoms of glaucoma acute attack dominated by strong headache and pain in the eye. Another common type of glaucoma is secondary glaucoma accompanying other eye diseases, such as inflammations, injuries or diabetes. Diagnostics
Diagnostics comprises four basic examinations: evaluation of the appearance of the optic disc, evaluation of the field of vision, taking the intraocular pressure and the assessment of the irido-corneal angle. The evaluation of the appearance of the optic disc is an element of the basic ophthalmic examination and should be performed as a stereoscopic examination by means of a slit lamp and Volka lens. A precise and comparable method of discovering loss in the field of vision is computer perymetry.
 There are different ways of taking intraocular pressure. The most common method is the use of Goldman applanation tonometer, but the most comfortable for the patient seems to be the use of a contactless tonometer. In this case, there is no contact between the apparatus and the eye surface, and the examination does not require any additional form of anaesthesia. We perform the examination of the irido-corneal angle by means of Zeiss or Goldmann goniolens. It allows the ophthalmologist to evaluate the risk of irido-corneal angle closure and discover its pathologies. Apart from basic forms of examination, there are additional techniques facilitating an early glaucoma diagnosis. Among others, they include confocal scanning laser ophthalmoscopy of the optic nerve (HRT II). The device performs 32 scans of the optic disc at different depths. Owing to this, a very precise determination of different parameters of the disc is possible, which can later be compared with values typical of the healthy eyes. It also makes it possible to discover even very small changes during subsequent control visits. Another important additional examination is the corneal thickness measurement, which allows us to calculate the real pressure prevailing in the eyeball, and consequently more precisely evaluate the risk of glaucoma progression.
There are different ways of taking intraocular pressure. The most common method is the use of Goldman applanation tonometer, but the most comfortable for the patient seems to be the use of a contactless tonometer. In this case, there is no contact between the apparatus and the eye surface, and the examination does not require any additional form of anaesthesia. We perform the examination of the irido-corneal angle by means of Zeiss or Goldmann goniolens. It allows the ophthalmologist to evaluate the risk of irido-corneal angle closure and discover its pathologies. Apart from basic forms of examination, there are additional techniques facilitating an early glaucoma diagnosis. Among others, they include confocal scanning laser ophthalmoscopy of the optic nerve (HRT II). The device performs 32 scans of the optic disc at different depths. Owing to this, a very precise determination of different parameters of the disc is possible, which can later be compared with values typical of the healthy eyes. It also makes it possible to discover even very small changes during subsequent control visits. Another important additional examination is the corneal thickness measurement, which allows us to calculate the real pressure prevailing in the eyeball, and consequently more precisely evaluate the risk of glaucoma progression. Treatment
 The aim of glaucoma treatment is lowering the intraocular pressure to such a level at which the progression of pathological changes does not take place any further. It should usually remain under 18,0 mmHg, which can be achieved through taking suitable eye drops diminishing the production of aqueous humour or increasing its outflow. If despite using two different antiglaucoma drugs the intraocular pressure remains high and the disease is progressing, a laser surgery or antiglaucoma operation should be considered.
The aim of glaucoma treatment is lowering the intraocular pressure to such a level at which the progression of pathological changes does not take place any further. It should usually remain under 18,0 mmHg, which can be achieved through taking suitable eye drops diminishing the production of aqueous humour or increasing its outflow. If despite using two different antiglaucoma drugs the intraocular pressure remains high and the disease is progressing, a laser surgery or antiglaucoma operation should be considered. Laser trabeculoplastics is a procedure during which focal photocoagulation of the trabecular meshwork is performed, which increases the outflow of aqueous humour from the eye. A good advantage of the surgery is the ease of performance, small risk of complications and the patient’s comfort, as it lasts for a short time and is performed as an outpatient service. The main disadvantage is the efficiency of the method, which is limited to the eyes with comparatively low rises of pressure and the positive effect proves transitory.
 Trabeculectomy is the most often performed surgery in connection with glaucoma. It consists in cutting out a fragment of trabecular meshwork together with the Schlemm’s canal creating a way of outflow of aqueous humour, which connects the anterior chamber of the eye with subconjunctival space. The surgery is highly efficient but it may involve numerous complications including cataract. To reduce the risk of complications, in some cases it is possible to perform a non-penetrating surgery, i.e. one in which there is no full-thickness eyeball opening. The most common procedure of that sort is deep sclerectomy with the use of absorbable scleral implant (SK GEL). In the case of closed-angle glaucoma it is vital to perform laser iridotomy, which consists in making a small hole in the iris for aqueous humour to drain from the posterior to the anterior chamber of the eye. This minor surgery in the majority of cases protects the patients from subsequent glaucoma attacks.
Trabeculectomy is the most often performed surgery in connection with glaucoma. It consists in cutting out a fragment of trabecular meshwork together with the Schlemm’s canal creating a way of outflow of aqueous humour, which connects the anterior chamber of the eye with subconjunctival space. The surgery is highly efficient but it may involve numerous complications including cataract. To reduce the risk of complications, in some cases it is possible to perform a non-penetrating surgery, i.e. one in which there is no full-thickness eyeball opening. The most common procedure of that sort is deep sclerectomy with the use of absorbable scleral implant (SK GEL). In the case of closed-angle glaucoma it is vital to perform laser iridotomy, which consists in making a small hole in the iris for aqueous humour to drain from the posterior to the anterior chamber of the eye. This minor surgery in the majority of cases protects the patients from subsequent glaucoma attacks. Preparation of the patient for the antiglaucoma surgery is similar to the one for cataract. One should remember that those surgeries should be performed as a matter of urgency.
STRABISMUS
Our specialists deal with diagnostics and non-invasive treatment of strabismus and amblyopia. There is a possibility of conducting a series of ortoptic and pleoptic exercises whose aim is the improvement of the eyeballs alignment and enhancing the visual acuity. Another method of treatment is laser retinal stimulation in the macular area.
If necessary, it is possible to implement surgical treatment of strabismus consisting in restoring the correct eye position. The surgery is performed in general anaesthesia administered by an experienced anaesthesiologist.
Patient’s preparation
During the qualification visit the patient is examined by an ophthalmologist and an anaesthesiologist. The patient is informed what medical examinations should be carried out and how to prepare for the operation.
- eating and drinking is not allowed 6 hours before the operation;
- if the patient takes any medications, they should be taken at the normal prescribed time;
- drugs ‘thinning’ blood should not be used within 7 days before the planned surgery after a consultation with an internist (i.e.: Acard, Acenokumarol, Polocard, Bestpirin);
We carry out diagnostics and treat such diseases as: dry eye syndrome, inflammatory diseases, and keratoconus.
Capsulotomy in capsule opafication, iridotomy and trabeculoplastics in glaucoma, photocoagulation in diabetic retinopathy and other retina diseases.
MINOR OPHTHALMIC SURGERIES
Within the eyeball 

- pterygium – the pathologically changed conjunctiva proliferates onto the cornea; the surgery consists in cutting out the changed tissue and closing the wound with the surrounding conjunctiva, if pterygiums are big and recurrent, the surgery should include the conjunctival graft,
- other conjunctival degeneration changes – for example: pinguecula, removed mainly for cosmetic reasons,
- pigmentation changes – clusters of pigmentation cells located on the eyeball, normally these changes are not dangerous, however some of them tend to become malignant so they should be removed without delay.
Within the eyelids
- yellow patches – (xantelazma) yellowish changes located near the inner canthus of the upper or lower eyelid, removed mainly for cosmetic reasons,
- warts - variously sized pathological skin changes, most often caused by viral infections,
- chalazion – a small bump caused as a result of an inflammation of the meibomian gland,
- entropion – a medical condition in which the eyelid folds inward usually appearing among older patients, it can lead to the damage of the cornea,
- ectropion – an age related medical condition in which the lower eyelid turns outwards and it causes excessive exposure of the eye,
Minor surgeries are performed under local anaesthesia. They last from several to several dozen minutes. After the removal of the changes the wound is stitched up and the stitches are taken out after 6-8 days. Depending on the character of the changes, in some cases the taken tissues are sent for histopathological examination.
Patient’s preparation
Before the surgery, the following examinations should be carried out: blood morphology, APTT, HBS, HCV. The the patient to be operated does not have to be on an empty stomach, patients with diabetes should stick to their normal rhythm of meals and insulin therapy. Before the operation the patient should not change the dosage of medications they take on everyday basis, however, drugs ‘thinning’ blood should not be used within 7 days before the planned surgery after a consultation with an internist (i.e.: Acard, Acenokumarol, Polocard, Bestpirin). Make-up should be washed off.
Additional examinations
 Fluorescein angiography - it consists in intravenous administration of a substance called: fluoroscein. It is a kind of dye capable of being fluorescent, which is recorded by a digital camera. It allows to visualise the damage and changes of the retina vessels. In order to perform the examination, it is necessary to dilate the pupil and inject in the vein under the elbow.
Fluorescein angiography - it consists in intravenous administration of a substance called: fluoroscein. It is a kind of dye capable of being fluorescent, which is recorded by a digital camera. It allows to visualise the damage and changes of the retina vessels. In order to perform the examination, it is necessary to dilate the pupil and inject in the vein under the elbow. Autokeratorefractometer (computer- aided visual examination) – automatic examination of visual impairment and the optic cornea power used routinely in ophthalmic examination, performed without touching the eye.

Biometry – measurement of the eyeball length and the eye structures performed under cornea anaesthesia with HRT II drops (Heidelberg Retina Tomograph). It allows to receive a three-dimensional picture of the posterior segment of the eye, and above all, of the optic disc. It provides a precise quantitative analysis of the optic disc, which has a special significance in glaucoma diagnostics and monitoring. The examination does not require any preparation, lasts several minutes and is carried out without touching the eye.
Pachymetry – an ultrasonic cornea thickness measurement, especially important in patients with glaucoma, corneal degenerations, or before a laser visual impairment correction and relaxing incisions. The examination is performed after anaesthetising the cornea with drops.
Field of vision – consists in the evaluation of the portion space visible at the moment of steady fixation of gaze in one direction. The computer examination of the field of vision is used in glaucoma diagnostics, pathological changes of the fundus and damage to the optic tract. The examination requires concentration and cooperation between the patient and the doctor. The patient sits in front of semicircular, illuminated cap of the apparatus and one of the eyes is covered. With the other eye the patient must constantly look at a light point at the centre of the cap and press the button held in the hand whenever another light point appears on the cap.
 Spectral Optical Coherence Tomography (SOCT) – records reflections of light from particular layers of the retina providing their cross-sectional images. It is the most modern way of macular diagnosis allowing the doctor to detect even small changes, which are still not seen in fluorescein angiography. The examination only requires pupil dilation.
Spectral Optical Coherence Tomography (SOCT) – records reflections of light from particular layers of the retina providing their cross-sectional images. It is the most modern way of macular diagnosis allowing the doctor to detect even small changes, which are still not seen in fluorescein angiography. The examination only requires pupil dilation. Applanation tonometry – intraocular pressure measurement
Cornea topography (mapping) – provides the evaluation of the topography of the anterior corneal surface in order to detect irregularities of the corneal surface. It is especially important in diagnostics and treatment of keratoconus and irregular astigmatism as well as in planning limbal relaxing incisions. The examination is carried out without touching the eye.
Ultrasonography (USG) – an examination providing the picture of the structure of the eyeball in the cases of optic opacities (leucoma, mature cataract, vitreous body hemorrhage) as well as in diagnostics of intraocular tumors and retinal detachment. The examination is performed through the eyelids with a bit of gel on top.




